Connect With Us
Blogs

Finding Relief From Foot Ulcers
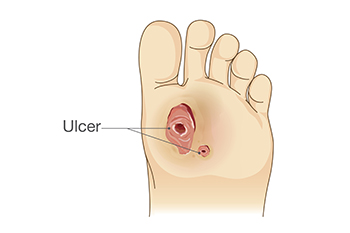
A foot ulcer is an open wound that develops on the bottom of the foot, often affecting individuals with diabetes or poor circulation. These ulcers are typically caused by nerve damage, prolonged pressure, and poor blood flow, which slow down the body’s natural healing process. Symptoms include pain, redness, swelling, and sometimes drainage or a foul odor, particularly when the ulcer becomes infected. Keep the wound clean and dry, and avoid putting pressure on the affected area for mild relief. Wearing proper footwear and using padded insoles can also help reduce pressure. If you have a foot ulcer, it is strongly suggested that you are under the care of a podiatrist who can treat foot wounds and help you manage any contributing underlying condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions please contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Are You Suffering From Ingrown Toenails?
Internal and External Causes of Cracked Heels

Dry feet, especially split heels, can result from both external and internal factors. External causes include prolonged standing, walking barefoot on hard surfaces, and wearing open-backed shoes that fail to support the skin. Exposure to dry air, harsh soaps, and excessive moisture loss can further weaken the skin’s protective barrier, leading to painful fissures. Internally, dehydration, vitamin deficiencies, and medical conditions like diabetes or hypothyroidism can contribute to skin breakdown. Poor circulation, which reduces the delivery of essential nutrients to the feet, can also make the skin more prone to cracking. If the cracks deepen, they may become painful or even infected. Keeping feet moisturized and wearing supportive footwear can help prevent and heel cracks. However, if deep fissures, pain, or signs of infection develop, it is suggested that you see a podiatrist for proper care and appropriate treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels may make you want to think twice about showing off your feet in warmer weather. However, cracked heels may be harmful to more than just the appearance of your feet. If deep fissures and cracks develop in your heels, they may make walking and standing painful for you. Additionally, these openings make way for germs to enter through your skin and cause infection.
There are several different causes of cracked heels. One of the most common reasons for this ailment is dry skin. This problem may make your keeps feel rough tight and itchy. Dry skin may be caused by cold air, extremely hot water, harsh soaps, and aging. Skin disorders such as eczema and psoriasis may eventually lead to dry skin. In some cases, complications may arise from cracked heels. Some of these complications are a loss of feeling in the heel, cellulitis, or a diabetic foot ulcer.
There are ways you can try to prevent getting cracked heels. One of the best ways to do so is to avoid wearing flip flops and sandals because these shoes increase your risk of drying out your feet. You should also avoid wearing shoes with a tall skinny heel, because these shoes cause your heel to expand sideways. At night, you should slather on a thick moisturizing cream on your feet and then cover them in socks to keep your feet moisturized overnight. Drinking water to stay hydrated is also a good way to ensure that your skin doesn’t become dry.
If you suffer from a severe case of cracked feet, you should make an appointment with your podiatrist to see what treatment methods are best for you.
Explaining Charcot Foot in Diabetic Patients

Charcot foot can develop in some people with diabetes as the result of peripheral neuropathy, which damages the nerves in the feet. This can lead to a loss of sensation, making it difficult to detect injuries such as fractures or joint dislocations. As a result, people may continue walking on an injured foot, causing further damage. Over time, the bones may weaken, leading to a collapse of the foot’s structure and significant changes in its shape. Symptoms of Charcot foot include swelling, redness, warmth, and a noticeable change in the shape of the foot or ankle. Without proper treatment, Charcot foot can increase the risk of foot ulcers, and, in severe cases, may require surgery or result in loss of limb. A podiatrist can assess the condition, provide immobilization options like specialized casts or braces, and recommend footwear to reduce pressure on the foot. In some cases, surgery may be necessary to stabilize the bones. If you are experiencing foot pain that may be related to peripheral neuropathy, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate reatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
Causes and Symptoms of Toe Cysts

A toe cyst, medically referred to as a myxoid cyst, is a fluid-filled sac that forms near the joints of the toes. They are typically located at the end of the toe or on the nail fold and may appear as small, soft, translucent bumps. These cysts are filled with a jelly-like substance that gives them a characteristic appearance. The primary symptom of a toe cyst is swelling and discomfort in the affected area. In some cases, it can lead to pain, especially when pressure is applied to the cyst. As the cyst grows, it can cause nail deformities and interfere with walking. The exact cause of a myxoid cyst is not entirely understood, but it is often associated with joint degeneration, trauma, or wear and tear on the toe. While the condition is typically benign, a myxoid cyst rarely shrinks on its own. For that reason, it is suggested that you consult a podiatrist who can monitor this condition and provide the necessary treatment.
Toe pain can disrupt your daily activities. If you have any concerns, contact Frederick Matthews, DPM of Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Types of Fifth Metatarsal Fractures

Fractures of the fifth metatarsal occur in various forms, depending on the location and cause of the break. The fifth metatarsal is a long bone located on the outer edge of the foot, connecting the midfoot to the base of the pinky toe. It plays an important role in maintaining balance, supporting weight, and enabling movement during activities such as walking, running, and jumping. Avulsion fractures, the most frequent type, happen when a tendon pulls a small piece of bone off the base of the fifth metatarsal. Dancer’s fractures, caused by twisting injuries, involve a diagonal break along the bone’s shaft. Stress fractures, resulting from repetitive activities like running, develop gradually and often affect the shaft or neck. Head and neck fractures of the 5th metatarsal typically occur from direct trauma to the bone. A podiatrist can use imaging tests to determine the type of fracture you have sustained. For guidance with a fractured foot bone, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and treatment options.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.