Connect With Us
Blog

Causes and Symptoms of Poor Circulation in the Feet

Poor circulation in the feet occurs when blood flow is restricted, often leading to discomfort, numbness, or a cold feeling. Causes include peripheral artery disease, diabetes, smoking, and a sedentary lifestyle. Risk factors include high blood pressure, high cholesterol, and obesity. Symptoms of poor circulation include tingling in the feet and toes, swelling, discoloration, or slow-healing wounds. These signs should not be ignored, as they may indicate more serious health conditions. A podiatrist can evaluate circulation, perform diagnostic tests, and recommend treatments such as compression therapy and lifestyle changes. If you experience persistent foot discomfort or signs of poor circulation, it is suggested that you consult a podiatrist for a thorough evaluation and personalized care plan to improve your foot health and overall well-being.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Frederick Matthews, DPM of Innovative Foot and Ankle Care. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
How Gait Affects Foot Health

Specific ways of walking, known as gait, affect how the feet, toes, and ankles bear weight. When pain appears in one area, such as toes, forefoot, midfoot, or heel, the body often shifts pressure to other areas without conscious effort. For instance, heel pain may lead to less pressure at the back of the foot but more under the forefoot. Pain in the arch can cause more force through the middle of the foot to maintain balance. If toes or the ball of the foot hurt, the push-off of each step becomes weaker causing other parts of the foot to take over. This can lead to discomfort in the feet or ankles. A podiatrist can carefully evaluate your gait, or walking pattern, identify where pressure is uneven, and recommend treatment to bring balance back to your foot function. If you have foot pain that may be related to changes in gait, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment.
If you have any concerns about your feet, contact Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
Cracked Heels Information

Cracked heels occur when the skin on the bottom of the feet becomes excessively dry and thick, leading to painful splits or fissures. Dry skin can be caused by prolonged standing, wearing open-back footwear, cold weather, or lack of moisture. Over time, the dryness may worsen and the skin loses elasticity, eventually leading to deep cracks that can cause discomfort, bleeding, or infection. Symptoms include rough patches, flaking, redness, and pain while walking. A podiatrist can assess the severity, remove thickened skin safely, recommend moisturizing treatments, and address any complications. If you are experiencing discomfort from having cracked heels, it is suggested that you schedule a visit with a podiatrist to restore smooth, healthy skin, and prevent further damage.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact Frederick Matthews, DPM from Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Causes of Foot Blisters on the Trail

Foot blisters while hiking are caused by friction, heat, and moisture building up between the skin and footwear. Common symptoms include redness, tenderness, and fluid-filled pockets. Risk factors include wearing ill-fitting shoes, sweaty feet, and long treks without breaks. Prevention involves wearing moisture-wicking socks, properly fitted hiking boots, and using blister pads or foot powders. Keeping feet dry and taking regular rest breaks can also reduce risk. If a blister becomes painful or shows signs of infection such as redness, swelling, or pus, it is important to seek medical attention. A podiatrist can clean and treat the area, prevent complications, and offer guidance for future hikes. If you have developed a foot blister that shows signs of infection, it is suggested that you consult this type of doctor who can safely treat foot blisters, and offer prevention tips.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact Frederick Matthews, DPM of Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
Adolescent Bunions and How They Are Treated
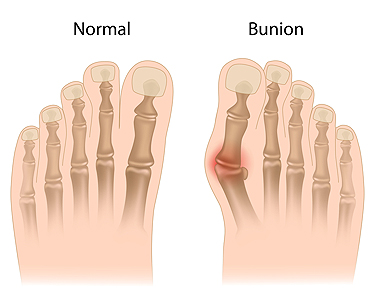
Bunions can affect teenagers, not just adults. A bunion is a bump that forms at the base of the big toe when the joint moves out of place. In adolescents, this often happens because of inherited foot structure or tight shoes. The condition may cause pain, swelling, or difficulty wearing certain shoes. Treatment usually begins with simple steps like changing footwear, using pads or cushions, and trying custom shoe inserts to ease pressure on the joint. If the bunion causes ongoing pain or affects walking, surgery may be considered. One option is a minimally invasive surgical technique that realigns the bone near the big toe joint using small incisions. It is often used in adolescents to correct bunions with less tissue disruption and faster recovery than open surgery. This allows for less disruption to the surrounding tissue and a quicker recovery. If your teen has a bunion that is not improving with conservative care, it is suggested that you see a podiatrist to explore the best treatment approach.
If you are suffering from bunion pain, contact Frederick Matthews, DPM of Innovative Foot and Ankle Care. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Plano, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.